All About Pain
 Key Points:
Key Points:
✓ Pain is the body’s warning system, alerting you that something is wrong.
✓ Acute pain is called ordinary or nociceptive pain. It protects us from hurting ourselves.
✓ Chronic pain refers to pain that has lasted for at least three months. It does not serve a useful purpose like warning us about something harmful.
✓ It may not be possible to eliminate all pain due to OI, but there are things you can do to reduce your pain.
In this module, you will read and see more about:
I. What is Pain ?
 Have you ever wondered why you feel pain? Pain is the body’s warning system, alerting you that something is wrong. Nerve cells, also called neurons, transmit signals from all the senses (e.g., touch, seeing, hearing…) including pain.
Have you ever wondered why you feel pain? Pain is the body’s warning system, alerting you that something is wrong. Nerve cells, also called neurons, transmit signals from all the senses (e.g., touch, seeing, hearing…) including pain.
Specialized pain neurons are found throughout the skin and other body tissues. When the pain neurons are stimulated, electrical and chemical signals travel through nerves in the spinal cord to the brain and are interpreted as pain.
Acute Pain
Acute pain is called ordinary or nociceptive pain. It is a useful sensation because it protects us from hurting ourselves. If we did not feel pain, we might burn our fingers on the stove or not know when we have a serious problem.
Acute pain is what you feel when normal nerves send messages to your brain from the injured body tissues. This is the type of pain you feel from a needle poke for blood work, or when you experience a fracture.
This pain is temporary, lasting minutes to several weeks. Acute pain goes away when healing occurs.
Chronic Pain
Chronic pain refers to pain that has lasted for at least three months. Unlike acute pain, chronic pain does not serve a useful purpose like warning us about something harmful. Sometimes with OI you can have chronic pain even without a fracture or due to an accumulation of microfractures from mechanical stress or bone deformities. Chronic pain can also result from delayed healing of an old fracture or surgery site.
Some kinds of chronic pain are not due to normal nerves reporting that tissues are injured or inflamed. Instead, these other kinds of pain, called nerve or neuropathic pain, are due to abnormal messages being sent to the brain by the nerves. This can happen even when the tissue is no longer inflamed or injured. For example, trigeminal neuralgia is a frequent source of neuropathic pain in OI and it is due to abnormal pain signaling from the trigeminal cranial nerve, leading to sudden, severe facial pain.
Nociplastic Pain
Nociplastic pain refers to pain that is caused by alterations in nociceptive signaling, but without a clear proof of tissue damage or nerve lesions.
The underlying mechanism for nociplastic pain is still not well understood, but scientists think it involves changes in the pain system, likely due to previous acute or chronic pain. You may be afraid of feeling pain again, leading to nociplastic pain.
How We Feel Pain
There are different reasons for why pain might persist, which help explain why pain may be experienced differently by two individuals.
Experts believe that there are many important reasons for why your pain might persist or differ from others, including:
- Your physiology, or the way your body is made up
- The way your body responds to physical and emotional stress
- Getting to school on time in the morning.
- The way that parents and friends respond to you
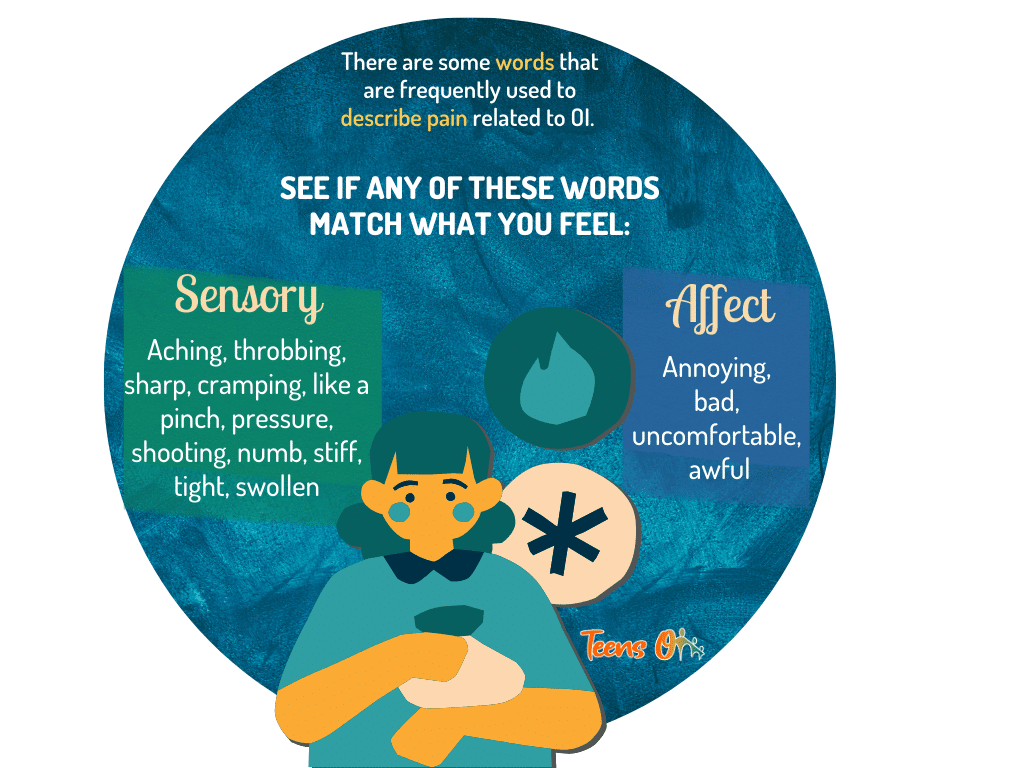
How to Communicate Your Pain
It is very hard to understand someone else’s pain since it is a very personal experience. It can be difficult for those around you to know how much pain you are experiencing when you may not have any visible signs of injury such as a cut, a bruise, or a small break in a bone.
Likewise, it is hard to describe to other people what your pain feels like. The use of pain-related words to describe your symptoms and feelings can help your family, friends, teacher, and healthcare provider better understand your condition.
Describing your Pain: Introducing “I’ve Got Pains”
“I’ve Got Pains”
by Karl William
I’ve got pain in my little finger,
It won’t go away.
No one to understand me,
“all pain is pain” they say.
But I’ve got some that seem to grow,
Take time, and build up slow.
I’ve got pains of every size.
I thought you should know.
Ol’ ‘Sally’, she’s a pain,
There when I wake.
And ‘Bert’, that little snake,
Follows my bones that break.
See, I have come to name,
All kinds of different pain,
And all I’m asking as I heal,
Is know which pain I feel.
Of all the pains that I feel,
Some break my heart.
Some words that people call me,
The jokes that tear apart.
Though I am strong you know,
A new smile is hard to grow.
And though an x-ray cannot tell,
My heart can break as well.
There are many ways to find out,
Just how I’m sore.
You’ve got the chart of faces,
Each hurts a little more.
There’s pain from one to ten,
A chart of words to describe me then.
But I don’t care which has appeal,
Just know which pain I feel!
[Chorus]
My will may be strong as steel,
But I proclaim the hidden pain I feel.
If you seek, maybe you shall find,
Which pain is on my mind.
Keep Track of Your Pain with a Pain Journal
It is important to keep detailed records of the pain you experienced or are currently experiencing. That way, the next time you have a medical appointment, you can share your pain diary with your doctor. Pain management specialists suggest writing three times a day – morning, noon and bedtime – at the same time every day, whether your pain is absent or present. If you’ve had a fracture and experience acute pain, this can be an added entry to your journal.
Here are some of the things you could keep track of in your journal:
Having a pain journal can help you and your health care provider identify the patterns and potential triggers of your chronic pain. Also, have a better understanding of what worked for you and what did not, and how your medication and therapy can be improved and tailored better to your needs.
When your pain is better controlled, you will see an improvement in your mood, be able to be more independent and go on to experience new things.
If you would like, you can download and print this pdf with 3 different pages to choose from and use as your Pain Journal.
Pain in Teens with Osteogenesis Imperfecta (OI)
Teens with OI may experience fractures that are accompanied by acute pain. Most teens with OI will encounter a few fractures during their lifetime. But some can experience multiple fractures as they grow if they are known to have Type III OI.
Chronic pain can also result from bone deformities, which form from previous fractures or during bone growth. When a fracture occurs, the body must repair the bone, but it does not always heal correctly even with medical treatment.
Adolescents with OI will often receive regular intravenous bisphosphonate treatment that will help get their bones stronger, decrease the amount of fracture and relieve the pain. Pain medications are another effective way to relieve pain, but it does not work for everybody. Some teens with severe forms of OI do not take analgesics because they do not experience significant pain relief with standard medication doses. Apart from medications, there are other ways to cope with pain. One example is using distraction tactics to keep your mind busy and avoid thinking about the pain. (adapted from the book The Dream Machine p. 44).
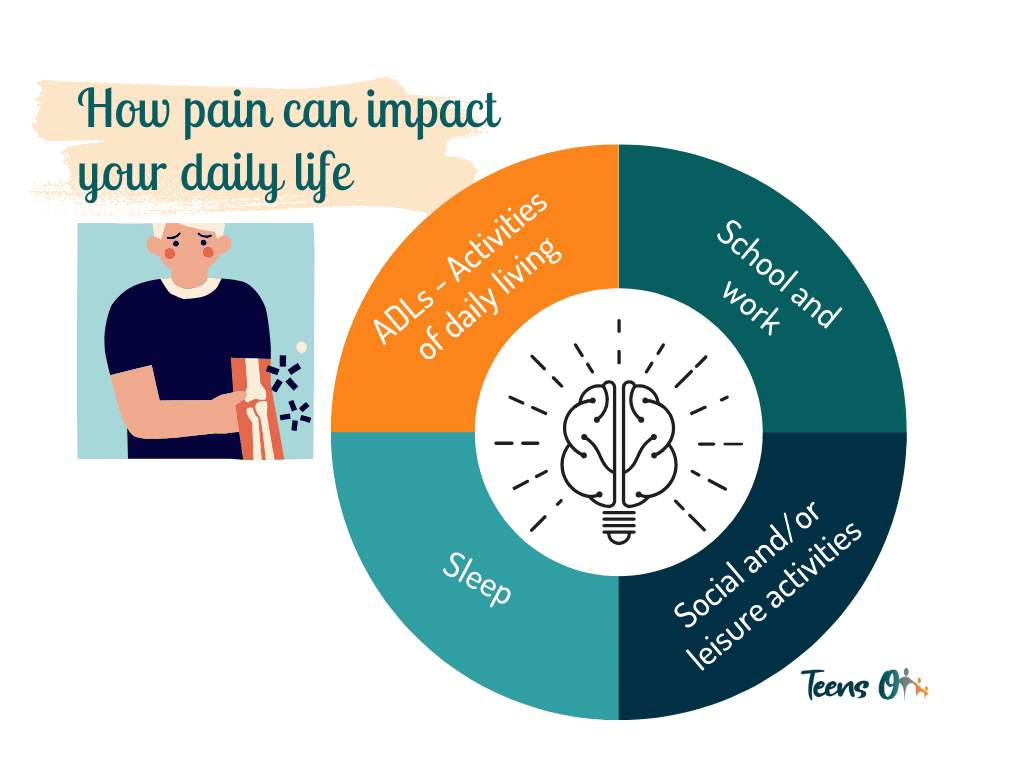
II. How Pain Can Impact your Daily Life
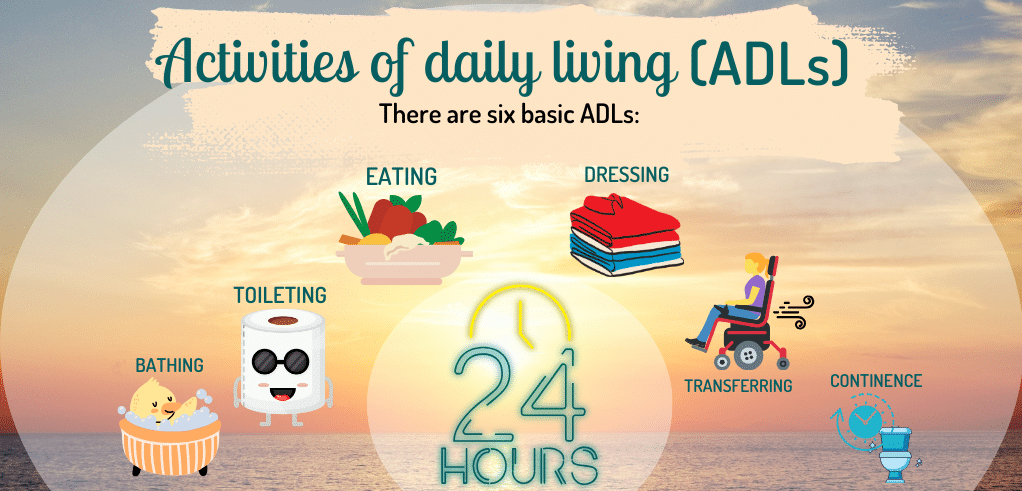
Activities of Daily Living
Activities of daily living (ADLs) are routine activities that people tend to do every day.
There are six basic ADLs: eating, bathing, dressing, toileting, transferring, and continence. The capacity to resume those ADLs can be compromised by pain.
Teens may sometimes need a walking or mobility aid like a walker, crutches, or a wheelchair. They may also need a wheelchair to help them move around when pain is too severe. Pain located in the joints makes it hard to fully move limbs or to stay in the same position. This can affect a person’s ability to climb stairs and sit for long periods of time. If pain is severe, individuals may require rest periods, which may also disrupt their normal daily routines.
Sleep
Sleep disturbances may also occur: it may be hard to fall asleep or you might find yourself waking up at night because of pain. This may affect school, work performance, and interfere with completing daily activities.
School and Work
When pain is too severe, teens may have difficulty getting to and attending school or work and completing their duties. Certain activities can increase pain; this is the case when lifting heavy objects or strenuous movements are involved. This may limit employment opportunities for some teens with OI.
Social and/or Leisure Activities
Opportunities for socialization or participation in sports can be restricted due to pain. If mobility is restricted due to pain, getting around to meet with friends may be difficult. Dealing with pain can also be energy draining – certain teens may feel like they have no energy left to socialize or participate in other activities after completing daily activities.
Research on Pain Associated with OI
Research on OI pain can help us determine some patterns among the pain experiences of people with OI, and help your health care team understand how to better approach the assessment and management of your pain.
Methods of Pain Assessment
Management of and research on pain starts with a good evaluation of your pain. The best method of assessment is what scientists call a “self-report” of pain. Pain is very personal experience, therefore it is important to obtain a report of what a person in pain is feeling in their own words using a structured approach. This is why you may hear your health care provider ask you to rate your pain on a scale of 0 to 10.
Sometimes, if the person who is in pain cannot use numbers or words to express their pain or have difficulty understanding the words, your health care provider may use other methods like complementary images to help gage your level of pain.
It is also important that different “dimensions” of pain are evaluated. The intensity of pain is only one of the many sensory dimensions of pain that health care providers can assess. Other elements of pain include: characteristics, location, duration, progression, as well as impact on physical, emotional and school functioning.
- Chronic Pain Can Persist into Adulthood
Children and teens with OI tend to experience pain that is associated with fractures and bone malformations as they grow. During adulthood, the number of fractures decrease, but acute and chronic pain can still be experienced. The pain is likely associated with having fractures and bone deformities from previous fractures. And despite different ways to control the pain (e.g. medications, wearing braces or finding ways to modify activities to avoid pain) chronic pain can still exist at mild levels.
Quality of Pain Research & Recommendations for Future Research
In general, the quality of OI pain research has been evaluated as low to moderate. This does not necessarily mean that the findings from these studies should be discarded. For example, some studies included young children in whom pain was very difficult to assess and researchers relied on the description of pain provided by parents. This is not the best method of pain assessment, but given the circumstances it might have been the only way at the time.
Research is ongoing and continues to look for solutions to help control your pain so that you can have an opportunity to live comfortably. Future researchers can help ensure high quality results when pain assessments follow the recommended criteria and being transparent how they conducted their research.
III. Pain Management Support System
Your Pain Can be Managed
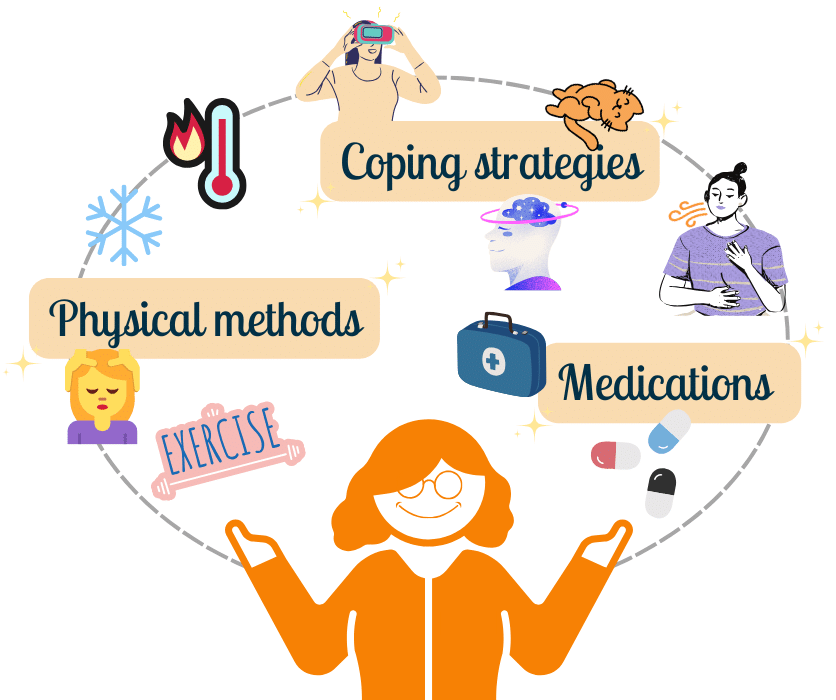
Pain can be changed by modifying pain signals from reaching your brain. These pain signals can be reduced or blocked anywhere along the pain pathway. This can be done using medications, physical methods and coping strategies. It may not be possible to eliminate all pain due to your OI. However, there are things you can do to reduce pain to levels that will let you do the things you want to.
⚙️ Pain can be managed using:
- Medications
- Physical methods such as heat, cold, massage, and exercise
- Coping strategies such as deep breathing, relaxation, distraction, and changing the way you think
Medications
Medications can help reduce your pain. You may already be taking medications to help control your pain. In this page, you will learn about common pain medicines that can help control pain.
The Teens OI – Managing OI online program – does not replace the use of the medications and treatments that your doctor has prescribed for you. It is important for you to learn about medications that can help reduce your pain. Speak to your doctor about these options and decide together if they are something you should try.
Types of Pain Medicines
Pain medicines are also called analgesics or painkillers. There are three main types of pain medicines:
- Non-opioids, such as Acetaminophen (Paracetamol) and Ibuprofen (NSAIDs, nonsteroidal anti-inflammatory drugs)
- Opioids, such as codeine and morphine
- Local and topical anesthetics, such as EMLA (lidocaine and prilocaine)
Mild Pain: Simple Analgesics
Simple analgesics, such as Acetaminophen and Ibuprofen, can relieve mild pain. Some mild pain relievers can be taken together if needed. However, you should not take ibuprofen if your doctor has prescribed another NSAID for you.
Topical analgesics, such as Diclofenac (Voltaren) can also help manage mild to moderate pain and, in some cases, can be used in conjunction with an oral pain reliever. The term “topical” refers to the route of administration, that is, topical agents are primarily applied directly to the painful area by rubbing it into the skin (e.g., creams, gels, sprays or patches).
Moderate Pain: Mild Opioids
For moderate pain, simple analgesics can be used with or without mild opioid medicines, such as codeine.
Severe Pain: Strong Opioids
For more severe pain, simple analgesics may be used with or without stronger opioid drugs, such as morphine.
These stronger pain medications are normally used for pain following a surgery or after a severe fracture. They are also used for some chronic pain conditions that do not respond to standard medical treatment. Strong opioid medications are not commonly used to treat pain in individuals with OI.
Like most medicines, opioids have side effects. It is important to discuss the benefits and side effects of any drug with your doctor, and to only use the medications as prescribed.
Local and Topical Anesthetics
Local anesthetics act on a specific part of the body. Lidocaine is a local anesthetic that is given by injection. Some local anesthetics are applied on the skin, in which case they are called topical anesthetics. Examples of topical anesthetics include EMLA cream and Tetracaine (Amethocaine). These anesthetics help to numb the surface of the skin. They can help reduce pain from needle pokes and other procedures.
Other Pain Medications
There are also some other medications that are used with special types of chronic nerve pain. These include tricyclic antidepressants such as Amitriptyline, and anticonvulsants such as Gabapentin. These medications help manage pain by decreasing the pain impulse from travelling in the nervous system.
How to Take Pain Medicines
- There is a right way and a wrong way to take medicine. The most common mistake people make when taking painkillers is not taking them soon enough. Most people wait until their pain is really bad before taking pain medicine. It is much easier to prevent pain from becoming unmanageable when you take the medicine early (when pain is mild) and regularly.
Medicine should always be taken according to the directions on the bottle or the way your doctor has told you. Too much medicine can cause serious harm. But, if you take less than the recommended dose, the medicine may not work.
- Pain medications work best when used in combination with physical and other pain coping strategies.
Bisphosphonate Treatment and Pain
Bisphosphonate treatment can help to build stronger bones for patients with OI. There is some scientific evidence that intravenous therapy of bisphosphonates may help with alleviating bone pain. However, most of the evidence we have is based on trials with adults where pain was not consistently measured. This makes it challenging for your health care providers to conclude with certainty that it will be useful for teens with OI. Thus depending on your situation, you might be offered this medical therapy.
Physical Methods such as Heat, Cold, Massage, and Exercise
Physical methods like heat, cold, touch, and exercise can help reduce pain.
These strategies can help improve your overall sense of well-being. They can improve your ability to do the things you want to do. Physical treatments can be used on their own for the treatment of pain. Usually, however, they are used in combination with other pain-relieving methods.
● Heat
Heat is helpful when dealing with pain due to stiffness. Applying heat increases blood flow. Heat feels soothing, and it can help relieve stiffness in your muscles and joints.
Here are some ways you can use heat:
- Use a heat pack or heating pad/blanket. You can replace the heating pad by placing rice or dry beans in a sock, knotting the top of the sock, and heating it in a microwave oven for 3 to 4 minutes.
- Rub on heating lotions or gels.
- Have a warm bath or shower.
- Do exercises in a hot tub or warm swimming pool.
- Use paraffin wax baths for your hands, feet, and elbows.
Be careful when using heat so you don’t burn yourself. Never fall asleep on a heating pad. Turn it off when you get sleepy.
● Cold
For some people, cold is a favorite way of dealing with pain. Cold gives a natural numbing effect. It numbs the nerve endings in the affected areas. Cold can also help to reduce swelling and inflammation by slowing blood flow and decreasing the activity of cells in your body.
Here are some ways you can use cold:
- Use a frozen gel pack wrapped in a towel.
- Try a plastic bag filled with ice or frozen vegetables (like peas or corn) wrapped in a towel to avoid freezing your skin.
- Use a cold cloth or compress.
- Rub on menthol-based gels or lotions.
Remember to be careful when using cold so that you don’t freeze your skin.
Heat and cold provide short-term pain relief. Some people find it helpful to alternate between using hot and cold for swelling, muscle spasms, and sore joints. Twenty minutes on and then 20 minutes off is a good rule of thumb when using both heat and cold.
● Massage
Massage or rubbing is another way to help manage pain. Massage can stretch and loosen stiff muscles and help decrease stress. Rubbing your sore joint will help to block the pain signals from reaching your brain.
Here are some ways you can use massage:
- Get a massage from a massage therapist, who is aware of your bone fragility.
- Give yourself a massage by rubbing the painful areas.
- Use a back-massage device or massage pillow.
● Exercise
Gentle, regular exercise can help protect your bones and muscles from further injury. Exercising can help build muscles, so that provide more support to your bones.
If a bone is surrounded by strong muscles, then there is less stress on the bone when it moves than if those muscles are weak and thin. Regular exercise can also help maintain your ideal weight which helps to reduce the pressure on your bones and joints.
Exercise encourages healing in injured or inflamed areas and can improve your energy level and mood. Exercise also releases your body’s own natural pain-relieving substances called endorphins.
It is important to find a type of exercise that you enjoy, like swimming, yoga, or walking your dog. You can build up slowly from there.
You might feel like doing nothing if you have pain and you cannot do your normal exercise routine. You may also want to be alone and just take it easy. This makes sense when you have pain that lasts a short time. However, with pain in the bones or joints that keeps coming back, you can end up spending too much time by yourself. This can lead you to feel lonely, down, and stressed out. Don’t let your pain keep you from doing the things you want to do, especially being with other people. After exercising, you may have a bit of muscle or joint soreness. A little soreness is normal, but severe soreness is a sign that you have done too much. It is important to push your body, but don’t exhaust yourself. If you have extreme soreness, reduce the intensity or length of the exercise and then gradually build up again. This is called pacing. It is better to pace yourself and give about the same amount of effort each day rather than do too much one day and nothing the next day.
Your doctor, nurse or physiotherapist can provide you with education and instruction on ways to stay active during a painful flare-up.
Coping Strategies for Pain
Pain coping strategies are very effective ways of dealing with pain and increasing your ability to do things. These strategies involve changing the way you think, feel, and behave in response to pain. These methods provide the longest lasting changes because they help your body’s own pain control system to work best. Practicing these methods over time can help change the way your pain signals are being sent to and from your brain. You may already know some of these methods and you will learn more throughout this section.
● Relaxation
Stress and pain can cause you to tense your muscles and hold your body in unusual ways. You and the people around you may not always notice this tension. The tension makes muscles tired because they are always held tight, instead of being loose and relaxed.
Learning how to relax can help you in many ways. You might be surprised at how learning such a simple skill can have so many benefits.
Relaxation can give you more energy, make you feel more alert and in control, and help:
- Reduce the effects of stress on your body, like anxiety and tension
- Manage the pain associated with a fracture by changing the pain messages
- Immobilize yourself, especially when coping with a fracture
- Deal with the decreased physical activity while waiting for a fracture to heal
- Think more clearly, concentrate, and remember things better
- Sleep better at night
- Enjoy things more
General tips for learning how to relax:
- Use your favourite, most comfortable chair or couch to practice the relaxation strategies you are about to learn.
- Don’t use your bed the first time you try out these relaxation strategies because you might fall asleep. Later on, you can use these strategies to help you fall asleep faster.
- Practice these exercises in a quiet place. You might need to put a sign up saying “Do Not Disturb – Relaxation in Progress.”
- Keep your legs and arms uncrossed. This will help your blood move through your body more easily.
- Practice these techniques every day to relieve stress. Use them at times when you are starting to feel pain or tension. Set a goal for how many times per week you will practice.
- Try doing the relaxation exercises at the same time each day.
- The more you practice, the better these techniques will work.
● Belly Breathing
Belly breathing is one of the best and easiest ways to relax. It is also called abdominal breathing. Breathing is an important part of relaxation, because our bodies need a constant supply of air to work smoothly.
When you breathe, you can use two different ways to breathe in. These are chest breathing and abdominal breathing.
Chest breathing is the way that we normally breathe. It is shallow, and can be fast. When you are stressed, your chest breathing becomes even faster. You might even feel short of breath. Shallow breathing makes your heart work harder to transport oxygen everywhere in your body. This extra effort can lead to other changes in your body like tense muscles and sweating.
Belly breathing is about breathing slowly and deeply, where air is drawn deep into the lungs and released. By breathing slowly and deeply, your body will receive enough oxygen and you can start to relax.
● Relaxation Using Tension
Relaxation using tension is a way to relieve muscle tension and pain by tensing and then relaxing different groups of muscles in your body.
It is suggested to start from your feet and work your way up to your head, or the other way around. This helps you relax further by guiding which group you should tense and relax next. After tensing the muscles for a few seconds, they will want to relax. You will be able to relax deeply after tensing your muscles. It is a good exercise to help you notice the difference between what tension and relaxation feel like. You can also achieve a state of relaxation by simply focusing on each part of your body whilst relaxing and letting go of whatever tension is there (see body-scan script).
● Relaxation Without Tension
- What it is and how it can help
You can learn to relax without tensing your body by imagining the feelings you have when your muscles are relaxed. This way, you won’t need to tense your muscles first.
- Learning How to Relax Without tension
As you did with the relaxation with tension exercise, find a comfortable, quiet place to sit. When you hit play on the clip, an audio recording will start. The audio recording will lead you through the muscle relaxation without tension exercise. Begin when you are ready.
- Practice Tips
- You need to put all of your focus and thought into this exercise.
- As you think about each muscle, you can let it get warm, heavy and relaxed.
- The relaxation gets deeper as you become familiar with the wonderful feelings of letting go.
- Letting your body relax gets easier each time you do it.
- Get comfy, sit back, and practice relaxing without tension.
- Enjoy the feelings of relaxation!
● Distraction
Remember that your brain perceives pain and there are ways you can change the pain signals or messages. Distraction is a technique you can use to change these pain signals. Distraction can help you to focus your attention onto other things rather than on the pain.
- Redirecting Your Attention
As we go through the day, our attention is constantly shifting. Sometimes we pay attention to a lot of things at once, but other times we get so caught up in a single thought or activity that we become less aware of what is going on around us.
Have you ever become so involved in one activity that you didn’t notice what was going on around you? For example, maybe you were playing a game and you didn’t hear your mom call you for dinner. Or perhaps you were really concentrating on a book you were reading and you didn’t notice the colour of the chair you were sitting in.
By focusing your attention on something else, you can block out unpleasant or stressful thoughts. By doing so, you will notice the pain less. The trick is to become as involved as possible in whatever it is that you are doing.
Here is an experiment you can use to try this technique:
- Focus your attention on your breathing. Notice how each breath moves your chest and stomach in and out. Notice how your breathing sounds, and how the air moves into your nose or mouth. Now begin to breathe more slowly. Take a deep breath in, and very slowly release.
- Immersing Yourself into a Virtual Reality
Virtual reality (VR) is a technology that brings someone into an imaginary world that looks and feels real. The imaginary world is created using advanced computer graphics and sounds. Using a headset and gamepads, you can move around and interact with objects in the VR world. Many different VR experiences exist, including watching cartoons, playing a game, going on an adventure, or travelling to a cool new destination.
VR can be used as a form of distraction when undergoing different medical procedures. For example, zoledronate treatment is given via an intravenous catheter (IV) poke, which may be painful or worrisome for some adolescents. To distract them from the IV poke, patients play a VR game. This helps them escape their worries and have fun in the virtual world. VR can also be used to help reduce anxiety and manage pain before and after surgery.
While VR can help you cope with pain and anxiety, it is not a medicine. VR may also not work for everyone. Some teens may prefer watching their medical procedure, listening to their music, or doing some deep breathing exercises. It is important you discuss with your nurse, doctor, or child life educator what options are available to you at the hospital to manage your pain and anxiety.
- Imagery
It is essential when experiencing pain to be able to bring comfort and calm to ourselves. Rather than tensing up and fighting pain, we need to cooperate with our bodies to create comfort by accepting and relaxing into pain. Stress produces shallow breathing and muscle tension which heighten pain sensation. So, we need to develop our capacity for deep breathing and muscle relaxation to break the cycle of pain, stress and heightened pain sensation.
We can also harness the power of our imagination to help diminish pain. The body has almost the same physiological reaction to an event that is imagined as to one that is actually experienced. So, if we think of something stressful, we will experience tension and, if we think of something relaxing, we will experience relaxation.
This is why it helps to describe pain in a neutral way. Here are two descriptions of an experience:
- I feel intense pain in my left foot
- My left foot is killing me.
The first description is merely the observation of a sensation that is being felt. The second is an emotionally charged interpretation likely to add to the stress of being in pain, and therefore also possibly heightening pain sensation. Since our thinking processes can affect the way we experience pain, it is important to use the power of thought to alleviate rather than heighten pain sensation.
The word imagination can be thought of in this way:
Imagination = Image in Action
This is because imagery does have a very active effect on the body. So, whilst practicing deep breathing and muscle relaxation, you can begin thinking of something that is very relaxing for you. A popular place to imagine is being at the beach, although of course you may choose anything else that you personally find relaxing. In order to completely immerse yourself in your imagery, it is helpful to involve as many of your five senses as possible. So, for example, if you are imagining being at the beach you could imagine hearing the sound of the water, seeing the blue sky, smelling the salt water of the ocean, feeling the warmth of the sun on your skin and tasting the ice cream you’re eating.
You can use any pleasant experience to help you relax. For imagery to work well, it should be easy to picture and calming for you. Practicing using our imagination in this way will help us build a reservoir of calm, an internal resource that we can call upon during those times we experience pain.
- Visualization
“This technique is similar to guided imagery. Visualization allows you to create your own images, which is different from guided imagery, where the images are suggested to you. It is another way of using your imagination to create a picture of yourself in any way you want, doing the things you want to do. All of us use a form of visualization every day – when we dream, worry, read a book, or listen to a story. In all these activities, the mind creates images for us to see. We also use visualization intentionally when making plans for the day, considering the possible outcomes of a decision we have to make, or rehearsing for an event or activity. Visualization can be done in different ways and can be used for longer periods of time or while you are engaged in other activities.
One way to use visualization to manage symptoms is to remember pleasant scenes from your past or create new scenes. To practice visualization, try to remember every detail of a special holiday or party that made you happy. Who was there? What happened? What did you do or talk about? You can also try this by remembering a vacation or some other memorable and pleasant event
Visualization can be used to plan the details of some future event or to fill in the details of a fantasy. For example, how would you spend a million dollars? What would be your ideal romantic encounter? What would your ideal home or garden look like? Where would you go and what would you do on your dream vacation
Another form of visualization involves using your mind to think of symbols that represent the discomfort or pain felt in different parts of your body. For example, a painful joint might be red or a tight chest might have a constricting band around it. After forming these images, you then try to change them. The red color might fade until there is no more colour, or the constricting band will stretch and stretch until it falls off; these new images then cause the way you think of the pain or discomfort to change.”
Reference:
Lorig, K., Holman, H., Sobel, D., Laurent, D., González, V., & Minor, M. (2013). Living a healthy life with chronic conditions: for ongoing physical and mental health conditions (4th ed.), Visualization (pp. 78, 81). Boulder, CO: Bull Publishing Company.
- Mental Games
Mental games are a way of controlling stress or pain by turning your attention away from stressful feelings. They involve using your mind to concentrate on a game. Your mind is thus occupied with another activity and therefore not available to dwell on pain or stress.
You may have already played these games to help pass the time during a long road trip. Here are some examples of mental games.
- Alphabet games. To play, think of any categories of interest, like sports, cars, teams, animals, or countries. Let’s say your category is countries. Think of a country that starts with the letter A, then B, C, and go all the way through the alphabet to Z.
- Try to remember all of the words to your favourite song.
- Count the number of tiles on the floor or dots on an area of the ceiling.
- Count backwards from 100, by any number you choose. For example, count backwards from 100 by fives. 100, 95, 90, 85…etc. until you get to 0.
- Look for faces or animals in the clouds.
- Participating in Activities
Participating in an enjoyable and distracting activity can help take your mind off the pain. If you are in pain, try to keep yourself busy with another task. It will distract your mind from the pain for a little while. Distracting activities can include:
- Talking to a friend on the telephone
- Playing a video game
- Reading a magazine
- Watching a movie
- Listening to music
- Baking a treat
- Working on a project
- Colouring a 🔗 mandala (download the pdf file)
- Creating an origami
- Prayers and Spirituality
“There is strong evidence in the medical literature of the relationship between spirituality and health. Spirituality is the way we can find meaning, hope, comfort, and inner peace in our lives. Many people find spirituality through religion. Some find it through music, art, or a connection with nature. Others find spirituality in their values and principles.
Many people are religious and share their religion with others. Others do not have a specific religion but do have spiritual beliefs. Our religion and beliefs bring a sense of meaning and purpose to our life, help us put things into perspective, and set priorities. Our beliefs may help us find comfort during difficult times. They can help us with acceptance and motivate us to make difficult changes. Being part of a spiritual or religious community offers a source of support when needed and the opportunity to help others.
People who belong to a religious or spiritual community or who regularly engage in religious activities, such as prayer or study, have improved health. There are many types of prayer – any of which may contribute to improved health: asking for help, direction or forgiveness; offering words of gratitude or praise; or giving blessings, among others. In addition, many religions have a tradition of contemplation or mediation. Prayer does not need a scientific explanation. It is probably the oldest of all self-management tools. Although religion and spirituality cannot be “prescribed”, we encourage you to explore your own beliefs. If you are religious, try practicing prayer more consistently. If you are not religious, consider adopting some form of reflection or meditative practice.
Also, if you are religious, consider telling your doctor and care team. Most won’t ask. Help them understand the importance of your beliefs in managing your health and life.”
Reference:
Lorig, K., Holman, H., Sobel, D., Laurent, D., González, V., & Minor, M. (2013). Living a healthy life with chronic conditions: for ongoing physical and mental health conditions (4th ed.), Prayer and Spirituality (pp. 82-83). Boulder, CO: Bull Publishing Company.
- Changing the Way You Think
You can reduce your stress or tension by changing some of the ways you think. Thinking positive is important, especially when you are feeling pain or recovering from a fracture. Negative thoughts and unrealistic beliefs, such as thinking that things are worse than they really are, can lead to stress, which can make symptoms worse.
Watch the French version here https://youtu.be/xncQXWO8N5s
IV. Complementary or Alternative Therapy
What are complementary or alternative therapies?
The terms ‘complementary medicine’ or ‘alternative medicine’ are used inter-changeably with traditional medicine in some countries. These terms refer to a broad set of health care practices that are not part of that country’s own tradition and are not integrated into the dominant health care system”. An example might be using acupuncture in addition to your medication.
- Talk to your doctor before starting any complementary or alternative therapies (CAM). You still need to take your prescribed medications.
Different Types of Complementary and Alternative Medicine (CAM)
● Whole Body System CAMs
Some CAMs address the whole body and how it works in health and disease. Examples of whole body system CAMs are:
- Naturopathic medicine: This is the use of natural, non-medical remedies to treat illnesses. It supports the body’s own healing ability using an integrated approach to disease diagnosis, treatment and prevention.
- Homeopathic medicine: This is the treatment of illnesses using very small doses of substances such as plant, mineral, or animal extracts. Traditional Chinese medicine includes a range of traditional medical practices that started in China over several thousand years ago. These practices include acupuncture, herbal medicine, and massage and Qigong (a type of exercise).
- Ayurveda: This is the world’s oldest science of healing that originated in India.
- Mind-body medicine: This includes meditation, word, sound and prayer.
- Manipulative practices: This includes chiropractic, osteopathy, and massage. Because of bone fragility associated with OI, these practices need to be tailored to your condition.
- Chiropractic treatments focus on adjusting the spine and manipulating the other joints and soft-tissues.
- Osteopathy is a manual examination and treatment method of the integrated musculoskeletal, visceral system and craniosacral systems. The osteopath examines and treats manually the mobility of all these systems and looks for limitations in mobility that could be linked to the patient’s complaint.
- Energy medicine: This includes energy field and bioelectromagnetic-based treatments such as magnets. Energy therapies focus on the energy fields thought to exist in and around the body.
● Dietary Supplements
A dietary supplement contains ingredients to add to the diet. These ingredients may be vitamins, minerals, herbs or other plant materials, amino acids, or enzymes. Supplements may come in pill, capsule, powder, or liquid form. They may be sold in a grocery, health food, or drug store. You can also get them through the internet, TV, or direct sales.
However, many supplements claim to treat or even cure. Unfortunately, there is usually no scientific evidence to support these claims. Always use caution when choosing a dietary supplement. You may want to check with a health care professional, such as a doctor, pharmacist, or dietitian, before taking any supplement.
Some dietary supplements have been proven effective. For example, vitamin D is important for building strong bones because it increases the absorption of calcium. When possible, try to prioritize getting nutrients from the food you eat as it contains other important molecules that will increase the absorption or increase the positive effects of those nutrients. However, when this is not possible, supplements are a great plan B!
● ‘Natural’ Doesn’t Always Mean ‘Safe’
There are many safe and effective supplements that come from natural sources like plants. Many traditional medicines also come from natural sources! However, ‘natural’ does not always mean ‘safe.’ Natural products can have side effects too. For example, there are mushrooms that grow naturally and are poisonous!
Dietary supplements may be regulated as ‘foods.’ They do not need to meet the same safety and effectiveness standards as medications do.
Some supplements have caused harm to people. The herbs kava and comfrey have caused severe liver damage. Supplements can be toxic or dangerous. A supplement can be contaminated with heavy metals, prescription drugs, or pesticides.
A supplement may interact with other medications you are taking. Studies have found that many bottles of commonly available supplements:
- did not contain the ingredients listed on the label,
- had very little of the active ingredient, or
- were contaminated with other dangerous compounds.
Evaluating Complementary and Alternative Therapies
If you are using or considering complementary or alternative therapies, talk to your doctor or nurse. Some of these therapies may interfere with your standard medical treatment.
● How to Get Reliable Information About a CAM Therapy
Find out what scientific studies say about the therapy you are interested in. Don’t take a CAM therapy simply because you saw it in an advertisement or on a Website. Don’t just take a CAM therapy because someone told you that it worked for them. Find out whether scientific studies support the claims made for that therapy.
Learn about the scientific evidence of the treatment’s risks, and potential benefits. This is critical to your health and safety. Scientific research on many CAM therapies is relatively new. This kind of information may not be available for every therapy. However, many studies on CAM treatments are under way. Our knowledge and understanding of CAM is increasing all the time. To find out more about current CAM therapies, check out the National Centre for Complementary and Alternative Medicine website: http://nccam.nih.gov/health/decisions/
● Before Trying CAM Therapy
Ask your doctor before trying CAM therapies. What works for someone else might not necessarily work for you.
- Do your research. Find out if there is scientific evidence about the effectiveness of the treatment. Also find out about any side effects. Get as much information as you can from independent sources. Don’t rely on those providing the treatment.
- Find out about the person giving the treatment. What kind of training does he or she have? How many of these treatments has the person performed? Does the practitioner belong to an organized group of some kind?
- Find out how much the treatment will cost. Also see if your insurance will cover it.
- Beware of alternative medicine practitioners who say they can cure diseases that do not respond to standard medical practice.
You might think that your doctor doesn’t want you to try CAM therapies. Because of this, you might feel uncomfortable telling your doctor. But it’s important for your doctor to know about all the treatments you are taking. Some CAM therapies can interfere with conventional treatments. Keep your doctor informed. It will ensure that you get the best care.
References:
Nghiem, T., Chougui, K., Michalovic, A., Lalloo, C., Stinson, J., Lafrance, M. E., Palomo, T., Dahan-Oliel, N., & Tsimicalis, A. (2018). Pain experiences of adults with osteogenesis imperfecta: An integrative review. Canadian journal of pain = Revue canadienne de la douleur, 2(1), 9–20. https://doi.org/10.1080/24740527.2017.1422115
Nghiem, T., Louli, J., Treherne, S. C., Anderson, C. E., Tsimicalis, A., Lalloo, C., Stinson, J. N., & Thorstad, K. (2017). Pain Experiences of Children and Adolescents With Osteogenesis Imperfecta: An Integrative Review. The Clinical journal of pain, 33(3), 271–280. https://doi.org/10.1097/AJP.0000000000000395